India struggles with the challenges of both Communicable and Non-Communicable diseases (CDs & NCDs). NCDs account for nearly half of the deaths in the country. The estimated economic burden of these ailments is close to $6.2 trillion (2012-30). CDs, maternal, antenatal and nutritional disorders constitute 40% of deaths in India.
Poor access to basic healthcare is a major cause rural of concern in India. Over 70% of India’s population is rural, whereas 80% doctors and 60% hospitals are in urban areas. Quality healthcare is sought very late in the disease cycle. Up to 80% of health care financing is out-of-pocket, and millions of households fall below poverty line every year due to their health care expenditures alone. Attempts of taking doctors to the rural areas have failed. Villagers are left to be treated by unqualified rural providers.
Telemedicine is one mechanism to bridge this healthcare gap and has been in existence for a number of years. Have you ever talked to your family doctor on the telephone? Well, that is also telemedicine!! Over the past few years, it has transformed into e-Health and m-Health, with rapid spread of Internet access and mobile connectivity, even in the tier-II and tier-III towns and cities.
For any technology to effectively address the needs of population at the bottom of the pyramid, following factors have to be kept in mind.
Affordability: Statistics show that the rural patients spend as much as 1.5 times their urban counterparts to access care for the same ailment. This is due to the expenses on travel, loss of wages, etc. If any technology based solution has to bridge the access gap for the rural population, it should be affordable for the rural population.
Accessibility: Nearest healthcare facility in the rural areas is located about 5-10 Kms away. Any proposed solution should be made available at a distance less than what the patient currently travels to meet a “Healthcare Provider”.
Quality: There can be no compromise on the quality of healthcare provided to the rural patient irrespective of any other factors. People demand, and justifiably so, good quality of care. Devices and Software should adhere to the international standards of quality or as prescribed by the local regulations in the region of operation.
Training: Any personnel, who are expected to use the innovative technologies, should not be expected to be highly qualified. With minimal training, they should be able to provide good care to the patients.
Under-medicalisation: There is a paucity of doctors in the rural areas and that need is not going to get addressed any time soon. Social Enterprises working in the healthcare industry should create solutions that depend on health workers who are already available in the region e.g. ANM, ASHA, etc. Skills of these health workers should be enhanced through the use of innovative technologies so that they are able to address the primary healthcare needs of the population. However, just creating technology solution is not enough. It also requires policy changes at the government level to allow such personnel to provide primary care, albeit after appropriate training.
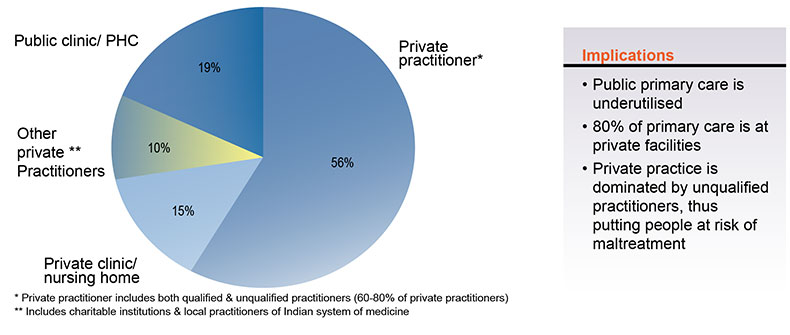
Fragmented Ecosystem: Only about 20% of the healthcare infrastructure in the country is public. Remaining is private, but majority of it is also disjointed and unorganized, especially in the semi-urban and rural areas.
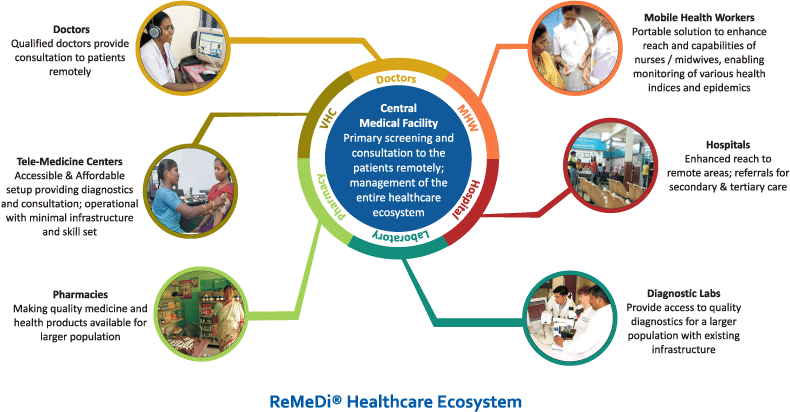
Any Social Innovation looking to address the healthcare needs should bring together the providers of various services – from consultation to diagnostics to medicines to referrals. ReMeDi® solution from Neurosynaptic is an example of a Social Innovation trying to bridge the gap between the rural population and the urban healthcare service providers by interconnecting various components of the healthcare ecosystem, and has been able to reach to over 5 Crore population with 2000 village health centers and over 8000 health workers, working at minimal infrastructure and bandwidth needs.
Infrastructure: Minimal infrastructure requirement for the solution.
Collaboration & Integration: Amongst technology and service delivery, among public and private sectors, alignment of funding supports for appropriate technologies and delivery, etc.
A number of Social Enterprises have been creating innovative products and technologies to address the needs of the population, who have till date been deprived of access to even the basic healthcare facilities. Some of these enterprises have created medical devices to enable health workers to carry out diagnostic tests at the point-of-care e.g. Biosense, Achira Labs, Bigtec etc. There are many others who have developed mobile applications to capture demographic and medical data for rural population e.g. PATH, D-Tree, etc. Quite a few organizations have been working in the rural areas to deliver healthcare services using technology e.g. World Health Partners, WISH Foundation, Meenakshi Mission Hospital, etc.
Last-mile technology-based health delivery through a well-integrated ecosystem has its own challenges, which are way different from the traditional usage of telemedicine technologies in the western world. With a large pool of social innovators and a readymade platform to deploy the innovations in the market, future looks really bright for healthcare delivery in India.
Source: BIRAC i3 – December 2015. Page 18 & 19